Should You Get a Gut Health Test? Why This Dietitian Doesn't Recommend Them (Yet)
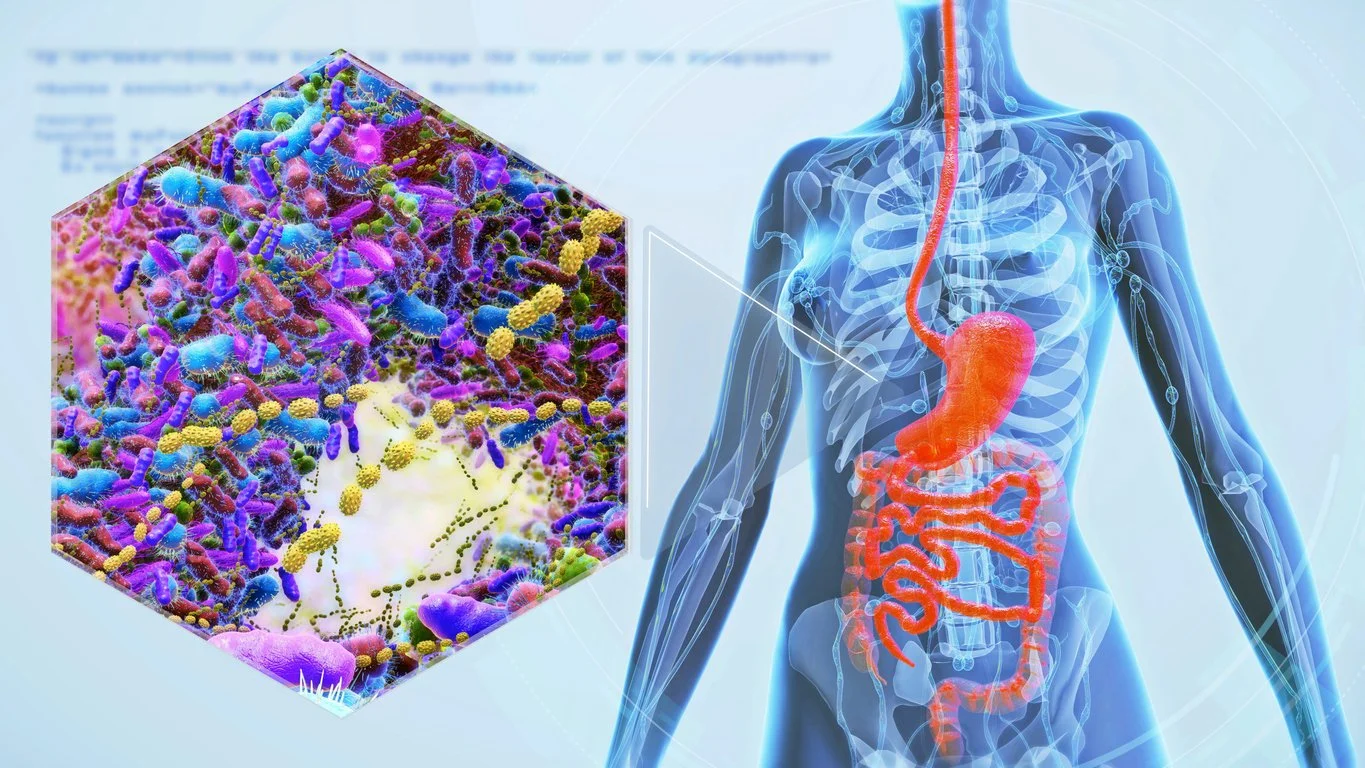
If you've ever wanted to take a gut health test, you're not alone. Gut microbiome tests are everywhere right now, promising to identify the "bad" microbes, explain why you're always bloated, and tell you exactly what to eat for better health. But are they all hype?
It's an appealing idea: Send in a stool sample, get a personalized report, and finally solve your gut issues once and for all. As a dietitian who specializes in gut health, I understand the excitement. Gut health plays a powerful role in everything from digestion and immunity to skin and mental health. It's no wonder people are looking for answers.
But here's the reality: While the gut microbiome is fascinating and important, the science around microbiome testing is still evolving. At the moment, these tests are more useful for research than for making specific clinical decisions. Plus, the results often raise more questions than answers, and in some cases, they can cause confusion and unnecessary dietary restriction.
That's why I'm writing this post. As a GI-focused dietitian, I believe in science-backed, practical approaches to improving digestive health, and right now, I'm not convinced that microbiome testing is the best tool for the job. Let's take a closer look at why.
What Are Gut Health Tests, and Why Are They Trending?
Gut health tests, often called microbiome or stool tests, analyze the microorganisms in your gut to provide insights into your digestive and overall health. They're trending thanks to growing interest in personalized wellness, social media buzz, and the promise of uncovering hidden causes of symptoms like bloating, fatigue, or food intolerances.
Understanding the basics
Gut microbiome tests are typically stool-based assessments (i.e., you send in a sample of your poop) that analyze the types and amounts of bacteria, fungi, and other microbes living in your gut. They aim to give a snapshot of your gut ecosystem, which plays a key role in functions like digestion and immune system regulation.
Many companies market these tests with the promise of highly personalized health solutions, like custom nutrition plans, targeted probiotic supplements, or food recommendations based on your unique microbiome profile. The idea is appealing, but in reality, the science is still catching up.
Common testing methods
Gut microbiome tests rely on different types of DNA sequencing and molecular biology techniques to analyze the microbes in your stool sample. Here are some of the most commonly used methods:
16S rRNA Sequencing: This method targets the 16S ribosomal RNA gene (a type of genetic material found in bacteria). It helps identify and classify bacteria down to the genus level by comparing gene sequences to reference databases. It's cost-effective and widely used, but it doesn't detect fungi or viruses, and it typically can't identify down to the species or strain level.
Quantitative PCR (qPCR): This targeted method amplifies and measures specific DNA sequences of interest, such as certain bacterial strains. It's highly sensitive and can measure microbial abundance fairly accurately. Still, it only detects what the test is designed to look for, so it may miss broader shifts in microbial diversity.
Shotgun Metagenomic Sequencing (Whole Genome Sequencing): This comprehensive method sequences all the genetic material in a stool sample, including bacteria, fungi, viruses, and other microbes. It offers a detailed snapshot of the entire microbiome and potential microbial functions, but it's more expensive and data-intensive than other methods.
Many popular gut health tests use one or more of these techniques to generate personalized reports. However, while the science is evolving, these methods vary in reliability, and their clinical usefulness remains limited. Plus, errors can occur at many steps during the testing process, from sample collection and DNA extraction to gene sequencing and data analysis.
The Science Behind Gut Microbiome Testing: What We Know (and Don't)
Despite their popularity, much of the science behind gut microbiome testing is still in its infancy. Here's a rundown of what we can currently measure using these tests (and what we can't).
What we can currently measure
Many gut health tests can identify which types of bacteria (and sometimes fungi and viruses) are present in your stool and estimate their relative abundance (basically, how dominant or rare certain microbes are in your gut ecosystem). However, even this information is sometimes inaccurate, with studies showing that different gut microbiome tests report different relative abundances, even when using the same stool sample.
What we cannot yet reliably interpret
Unfortunately, when it comes to gut microbiome tests, there's a lot of data we can't reliably interpret. Here are some areas where the science is still evolving:
Identification at the strain level and diversity measurements are still inaccurate: While some advanced tests attempt to identify microbes at the strain level, this isn't always consistent or reliable. One study found that when the same stool sample was analyzed using six different microbiome tests, some kits rated bacterial diversity as "excellent" or "good," while others rated it as "unfavorable" or "average." This indicates that the analytical methods being used are not accurate enough to provide this kind of information. In addition, bacterial diversity is rated compared to a "reference cohort." That means that the interpretation is dependent on the reference cohort's characteristics. Using a different reference cohort could lead to a completely different interpretation.
We don't currently have a clear definition of what a "healthy" microbiome looks like: While we know diversity and balance are important, there's no universally agreed-upon standard for what a healthy gut microbiome looks like, especially across different populations and health conditions. Plus, although we're starting to see associations between specific microbes and diseases, it’s hard to pinpoint whether the altered microbiome profile caused the disease.
The microbes in your stool may not accurately represent the microbes in your gut: Most tests analyze the microbes found in stool, but this doesn't always reflect what's happening throughout the entire gastrointestinal tract.
High individual variability: The composition of your gut microbiome is shaped by many factors, including genetics, diet, lifestyle, geography, and medication use. This makes it difficult to compare one person's results to a universal "ideal" microbiome profile.
Limited clinical relevance of strain-level data: Even when tests can identify specific microbial strains, we don't always know how they impact disease or symptoms. While there is some correlation between the human gut microbiome and diseases, the presence or absence of a particular microbial strain doesn't necessarily mean someone will experience specific health outcomes.
An interesting study published in 2024 used the same stool sample for six different microbiome tests. They found that the results received in each test's report differed, indicating that at least some of the test results were not accurate. The researchers concluded that these differences happened because the testing methods weren't clinically validated (i.e., not proven to work in real-world medical settings).
This is the current state of gut microbiome testing. While we can identify bacteria, fungi, and other microorganisms present in a sample, we don’t yet have the knowledge to interpret what their presence means in a way that reliably guides healthcare decisions. We don’t know which combinations of microbes are universally "good" or "bad," how they interact uniquely within each individual, or how external factors (like diet, lifestyle, and supplements) affect their role in health.
Until we unlock this "translation," making personalized treatment or nutrition recommendations based on gut microbiome tests is like prescribing a medical treatment based on an unreadable ancient text—speculative at best, and misleading at worst.
Why Gut Health Tests May Do More Harm Than Good
As much as I would love for gut microbiome tests to inform the care I provide to my patients, the reality is, the science just isn't there yet. Here are some of the downfalls of gut health tests that I frequently see in my practice.
Cost without clinical value
Gut microbiome tests are often not covered by insurance, meaning patients pay for them out of pocket (not just for the test itself, but also for interpretation, follow-up appointments, and recommended supplements). With limited evidence that these interventions improve symptoms, the return on investment is questionable.
Treatment fatigue and confusion
In my experience, many patients become overwhelmed and discouraged after trying to "fix" test results that may not even be clinically relevant. This can lead to unnecessary dietary restrictions, excessive supplements, and increased stress—ironically, all things that can worsen gut symptoms.
Compromised trust in care
When people invest time and money into a test and don't see any meaningful relief from their symptoms, it can erode their trust in the healthcare system and evidence-based providers. Some people may even turn away from conventional care entirely, delaying or avoiding proven treatments.
Supplement overload
Many gut health tests are directly tied to proprietary supplement lines (like pre- and probiotics), which can lead to overly complicated supplement regimens with a high pill burden. The financial costs add up quickly, and many supplements marketed this way lack strong clinical backing.
Why The Microbiome Still Matters, But Testing Isn't The Answer (Yet)
While the gut microbiome plays an important role in overall health, current testing methods aren't yet reliable or actionable enough to guide personalized treatment.
We need more research
The gut microbiome plays a crucial role in digestion, immunity, inflammation, and even mental health, but we're still in the early stages of understanding exactly how to harness this information in clinical practice. Current gut health tests outpace the science in terms of what we can meaningfully interpret and act on.
However, research is rapidly evolving, and gut microbiome scientists are exploring how specific microbes influence disease risk, how diet shapes microbial communities, and how interventions like pre- and probiotics can support gut health. One day, microbiome testing may help us tailor interventions to an individual's gut profile. For now, though, the tools we have just aren't there.
What actually supports gut health today
Until the science catches up, supporting gut health through foundational habits remains the best approach. Here are some habits that research shows support a healthy gut:
Eating a diverse, fiber-rich diet: Eating a variety of plant-based foods like fruits, vegetables, whole grains, legumes, nuts, and seeds, feeds different types of beneficial microbes. Diversity in your diet = diversity in your gut microbiome.
Including fermented foods: Fermented foods like yogurt, kefir, kimchi, and sauerkraut can introduce beneficial microbes and promote a healthy gut independent of their probiotic effects.
Prioritizing movement, sleep, and stress management: Regular physical activity, getting enough sleep, and managing stress all play an essential role in maintaining a healthy gut. Chronic stress and sleep disruptions can negatively impact the gut-brain axis and the gut microbiome.
Being consistent with healthy habits: Gut health doesn't hinge on a single food or supplement. It's built over time through steady, sustainable habits that are backed by evidence, not hype.
Working with a dietitian or GI specialist: If you're dealing with digestive symptoms like gas, bloating, and abdominal pain, start with a qualified provider. A dietitian can help identify patterns and triggers and offer practical, food-first strategies rooted in science.
Being wary of quick fixes: Despite supplements and tests that promise to heal your gut, there's no one-size-fits-all approach to gut health. Be wary of expensive tests and supplement regimens promising a cure-all. Gut health takes time, personalization, and a focus on the fundamentals.
Final Thoughts
Gut health is crucial to our overall well-being, but despite the growing hype, the gut microbiome tests currently on the market don't yet offer the clarity or direction they promise. While they may seem like the magic bullet to better health, they often fall short on clinical value and can leave you confused, frustrated, and overwhelmed.
Instead of chasing uncertain results, focus on well-researched habits that support a healthy gut every day. If you're experiencing gut symptoms, work with a provider who prioritizes practical, sustainable solutions over pricey quick fixes.
If you’re interested in working with a GI dietitian to improve your gut health, click here to book a free 15-minute discovery call with me - let’s chat!